
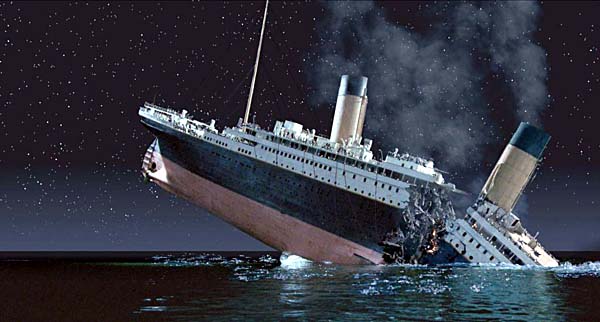
In my opinion and those of others who treat patients the new 2015 Dietary Guidelines for America (DGA) will not stall the Diabetes Epidemic and we continue Full Steam to the Full Catastrophe. But there are more runners now than ever before and exercise was going to fix all this stuff? You may not pay much attention to the DGA but millions of kids at school lunch, WIC programs, and the public’s perception of what is healthy trickles down from the DGA. As we have heard before fruits, vegetables, and whole grains are the foundation of a healthy diet. Fat was not even on the 2010 “My Plate” further ingraining an unfortunate homonym of dietary fat causing one to be fat (obesity).
The truth is often difficult to get to the surface but with persistence and dedication to the rigorous science the rock can move. For the first time in 35 years the Dietary Guidelines for America (DGA) received an independent review funded by Congress (not special interest). The petition shared on this site helped make this happen through The Nutrition Coalition which I am a member. http://www.nutrition-coalition.org
The Washington Post shared the story.
A few things are headed in the right direction. Two months ago the Coke Global Energy Balance Network was shut down by the verdict of scientific and public opinion. In the 2015 version of the DGA there was a strong emphasis for reducing sugar, eating cholesterol is no longer a concern, and eggs and coffee are off the black list. Healthier eating patterns are emphasized too centered around the usual fruits, veggies, beans/legumes, low fat dairy, and whole grains. Later in this post I’ll describe why this prudent advice is fine for a well person, but not for one who is Insulin Resistant.
A good summary of the 2015 DGA is from the Washington Post. Our group is mentioned at the end of the article . https://www.washingtonpost.com/news/wonk/wp/2016/01/07/government-revises-dietary-guidelines-for-americans-go-ahead-and-have-some-eggs/
In the process of challenging conventional wisdom our group was attacked by political action groups such as the CSPI who in this article calls us “Full of Baloney” . http://thehill.com/blogs/congress-blog/healthcare/257353-coalition-is-full-of-baloney-on-nutrition-guidelines
CSPI stands for Center for Science in the Public Interest however don’t be fooled by the name. They are a political action group in the service of their constituents. Read their reversal on Trans-fat here. https://www.washingtonpost.com/news/morning-mix/wp/2015/06/17/how-trans-fats-just-banned-were-once-touted-as-the-healthy-alternative/
CSPIs first stance was to tout the Trans Fats as the healthy alternative to Saturated Fats in a movement to shut down the Palm and Coconut Oil industries which were in the Pacific Islands and a threat to US producers of the new fast food, processed food, and baking darling. CSPI later reversed course to condemn the Trans Fats after tireless work of Dr. Fred Kummerow, who at age 100 and still publishing his work, finally had the impact to eliminate the toxic fat. For years Fred was voted off the nutrition island as he challenged the safety of Trans Fat in a Quixotic mission.
Here was CSPI leader Bonnie Liebman’s overhanded email to our group in response to a controversial but thoroughly referenced article of Nina Teicholz in the British Medical Journal (BMJ). Her efforts were trying to get us all to resign or our academic credibility would be sacrificed. The BMJ did not retract the article which can be read here http://www.bmj.com/content/351/bmj.h4962
Dear Nutrition Coalition members:
Yesterday, more than 180 scientists from 19 countries asked the BMJ to retract Nina Teicholz’s investigation of the 2015 DGAC’s Scientific Report.
Sincerely,
Bonnie F. Liebman, MS
Director of Nutrition
Center for Science in the Public Interest
Washington, DC 20005
One of the 180 signers was Dr. David Katz of Yale who made claims that Nina had conflict of interest because she wrote a book. Curiously Dr. Katz has 3 books to sell under his name and others under a pseudo name in the field of Science Fiction. Bizarrely he reviewed his own Sci-Fi work with glowing words from Dr David Katz for the Huffington Post. The Yale Daily News exposed the “illuminating” story. http://yaledailynews.com/blog/2015/11/04/katz-faces-criticism-for-book-review/
The call for retraction was also signed by one of the thought leaders of past nutrition guideleines and member of the DGA Advisory Panel Dr. Alice Lichtenstein of Tufts (http://www.nutrition.tufts.edu/faculty/lichtenstein-alice)
She dismissed the groundbreaking work of LDL subtypes by clinical and research leader Dr. Ronald Krauss before the 2010 version. Dr. Krauss is unique in this space. He, like myself, sees patients and is not merely looking at epidemiology spreadsheets and flawed studies from the hall of mirrors of nutritional science that are often argued as proof of principle for one’s position. A bit on Dr. Krauss here:
http://profiles.ucsf.edu/ronald.krauss
https://experiencelife.com/article/a-big-fat-mistake/
As Nina Teicholz shares in her book “Big Fat Surprise” Lichenstein’s was a leader to drive recommended levels of saturated fat below 7% of calories when evidence to any benefit of this was lacking:
When I asked Lichenstein whether her committee had considered Krauss’s work on LDL subfractions and their implication for saturated fat, she replied the work was “complicated” and that she “didn’t have the time” to review it.
This current publication is worth the read and gives a good summary of what are emerging areas of Cardiovascular Risk. Krauss was on it 15 years ago.
So where does this leave us as we go forward? My opinion which is based on the science and clinical experience of dealing with pre Diabetes (PreDM) and Diabetes (DM)- the majority of the country and even higher percent of people entering the medical clinics.
The DGA are for the uber well person who is not genetically programmed for Insulin Resistance and who has capacity to keep active . Sadly I see too many patients with Insulin Resistance who have no clue they have and steam on toward the Full Catastrophe. Many have progressed to full blown Diabetes before a health care provider has alerted them to change course, and even then the direction is not toward safety.
With the liberal amounts of sugar still allowed it is still “safe” to consume over 200 grams carbohydrates per day in a population where the majority of people are carb intolerant. In the guidelines sugar is recognized as dangerous, but yet a diabetic is allowed 10 added teaspoons per day. That’s 10 teaspoons of poison. Think if we still allowed as safe 10 cigarettes a day for an Emphysema or Lung Cancer patient. Remember it was not too long ago we did not connect tobacco to cancer or lung disease.
Saturated fat is still demonized when no evidence exists that it has any ill effects when part of a healthy real food diet. So if we look at the predicted metabolic and lipid effects of prudently following the current DGA recommendations we can expect to :
– Increase TG (bad)
– Decrease HDL (bad)
– Increase small dense LDL particles (very bad)
– Increase inflammation (bad)
– Increase oxidative stress (less Sat Fat = more PUFA)
– Increase obesity in the majority with Insulin Resistance and Carb intolerance
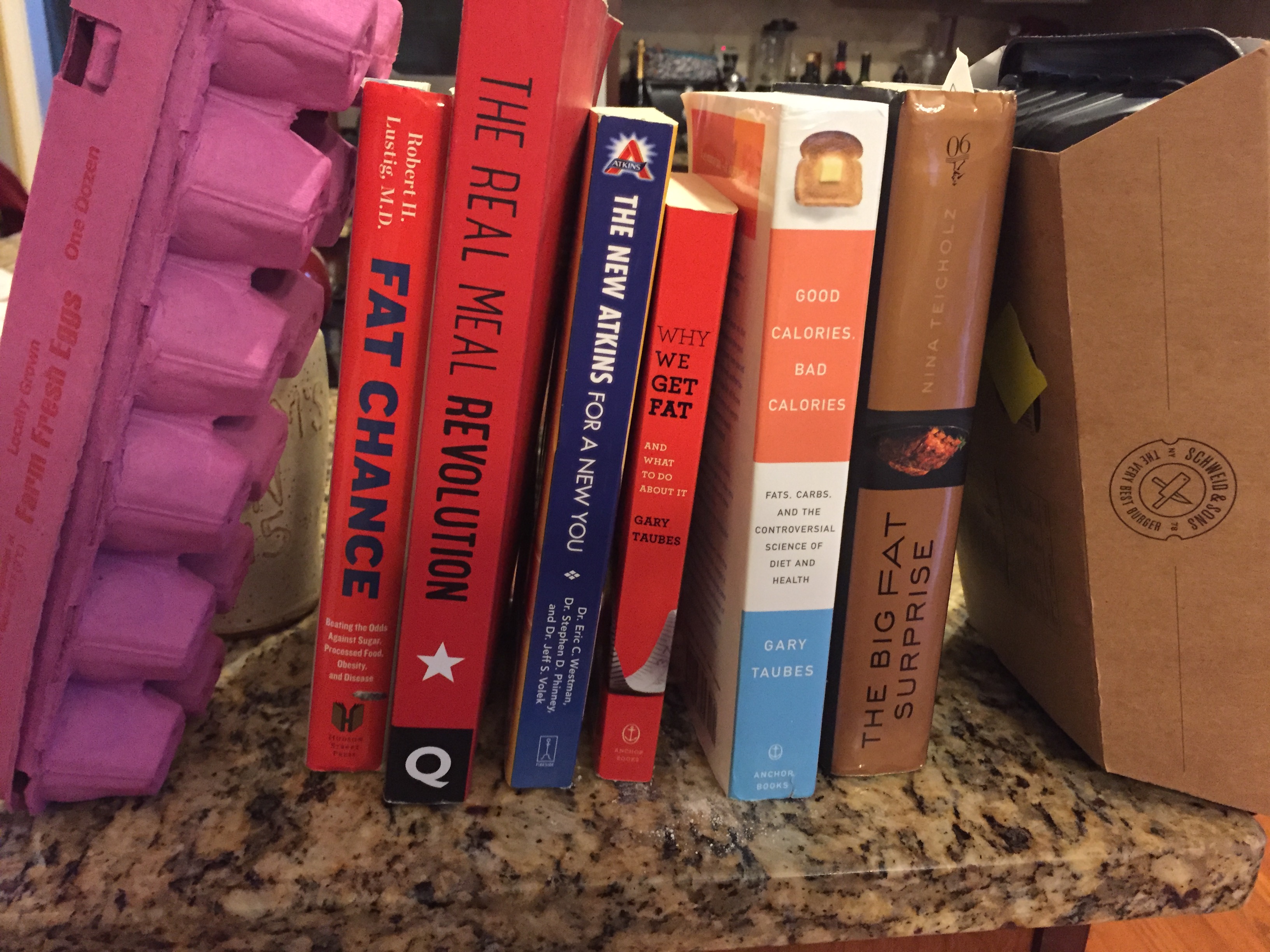
If this is confusion read the article linked above these paragraphs or for deep reads pick up “Good Calories Bad Calories” by Gary Taubes , “Fat Chance” by Dr Robert Lustig, or Nina’s book mentioned above.
The Key Books Held up by Farm Eggs and Grass Fed Beef packages
…………
So will the new DGA help us reverse course and sail to safe harbors? This is reversing pre Diabetes (PreDM) and Diabetes (DM) which are driving the Metabolic Syndrome which is the “Full Catastrophe” .
[what is the Metabolic Syndrome? http://www.nhlbi.nih.gov/health/health-topics/topics/ms ]
Supported by literature and human physiology is the need to be very specific on carb counts to reduce endogenous insulin and Insulin Resistance (IR). More insulin means more IR, so reversal is about specific carb tolerance (very low for pre DM and DM) and yet never be hungry. Healthy fat needs to be central. Fats do not raise glucose or insulin and are satiating. Better glucose control with more meds (those that increase insulin) leads to worse outcomes in the things that matter (Cardiovascular events, death).
Prudent guidelines work for well people, but not those with preDM or DM.
The handouts I use for patients can be found at http://tworiverstreads.com/simple-food-rules/ . The videos on “low carb 101” and “Dr Westman’s no sugar no starch” explain a lot. It is then up to health professionals and coaches to work with patients and individuals. We do this in our hospital. It is fun and patients get it. Never let patients be hungry. Tell them to throw out “energy balance” and let them off the hook. It is not their fault they have IR leading to DM. Gary Taubes 2008 book “Good Calories Bad Calories” is the tome. He lays it all out.
Our National Goal must be to improve health, reverse disease, and lower cost; not “intensify management”.
We must remember this – genes have no effect unless expressed.
Why does this matter? Eskimos and Native Americans carry genes for preDM and DM but never had this before modern diets. The genes were there but were not turned on. To reverse DM we must turn on other genes. Likely everyone reading this has genes for IR leading to preDM and DM if given right environment. I too have moderate IR.
Here a good article about how diabetics are different in cardiovascular risk counseling, much of it is about IR. “Type 2 diabetes and cardiovascular disease: Have all risk factors the same strength?” http://www.ncbi.nlm.nih.gov/pmc/articles/PMC4127581/
We use a term called “residual risk” which to the patient sounds like a scientific term about something that is residual, unchangeable, and is the way it is (like residue on your tub after the washing it). The reality is most have no idea what this means. The article shows the increased risk of cardiovascular disease and stroke in diabetics anywhere between two times up to eight times average risk. Even if we mitigate traditional risk factors, diabetics still have significant residual risk which is great. Physicians and patients just accept that is the way it is and the risk cannot be measured or affected outside of our usual “risk factor management”.
We still think our traditional ways of managing these risk factors make a difference and it is hard to reverse conventional wisdom. The largest trial done at its time called “MRFIT” went all in for the highest risk patients (many DM) on all risk factors that we thought important (exercise, smoking, HTN, sat fat). Read the results of this trial and there are several fascinating theories as to why it did not work, but we still believed in our ingrained ways. We wanted to believe. This journal club article summarizes it.
http://www.wikijournalclub.org/wiki/MRFIT
The theory that residual risk cannot be mitigated is just not true. You can mitigate the risk by reversing the diabetes and looking at other factors which objectively measure residual risk. Advanced lipid markers (LDL particle number and size) as well as the simple post meal glucose. Beyond the sugar and starch as driving the risk, other things to consider are the microbiome, Polyunsaturated Fats (PUFAs), and other yet to be discovered triggers of inflammation.
There is such individual variability that every preDM and DM should be checking their post meal glucose even if they are not on insulin. This is a clear marker of glucose intolerance, insulin resistance, hyperinsulinemia, AGEs (Advanced Glycated Endproducts), and inflammatory pathways which reflect residual risk.
Post meal sugar is so simple and telling. For example this week I was in Connecticut doing some work on filming running exercises. I went for an hour run early in the morning followed by a three egg Burrito (whole wheat wrap). It had avocado, cheese, and veggies in it too. I’d worked up an appetite! We proceeded to do two hours of mostly active work with running and filming and out of curiosity I checked my glucose with my glucometer. We know pre meal and post meal exercise helps insulin sensitivity so this should be a good reading.
At nearly age 50 I am partially insulin resistant and have the genetic programming to turn on this gene if the environment allows it to happen. The only way genes get turned on is if they have an environmental cue (the term is epigenetics). My glucose two hours after even the fairly low carb high fat meal in a scenario where my insulin sensitivity is optimized from exercise still reflected a glucose of 125. Now just imagine if even someone like myself who is “well” did not exercise before breakfast, had three muffins, and then sat at a desk. I don’t want to do this experiment but I might just to see what the two hour post meal glucose would be. A preDM or DM person who does similar will likely be off the charts even though the sugar might reset by the next morning and a false assumption that all is well.
Just food for thought as we teach our patients to learn their bodies and individualized their management which in essence is treating their food and activity patterns to reduce all hyperglycemia and insulin loads. Simple way- get a glucometer (30 bucks WallMart)!
Hot off press this week also:
CONSENSUS STATEMENT BY THE AMERICAN ASSOCIATION OF CLINICAL ENDOCRINOLOGISTS AND AMERICAN COLLEGE OF ENDOCRINOLOGY ON THE COMPREHENSIVE TYPE 2 DIABETES MANAGEMENT ALGORITHM – 2016 EXECUTIVE SUMMARY
https://www.aace.com/files/aace_algorithm_slides.pptx
https://www.aace.com/sites/all/files/diabetes-algorithm-executive-summary.pdf
A few moves in the right direction from the Specialty Managing (but not reversing) Diabetes.
- Mention LDL particle number as important
- Apo B important
- #1 intervention is lifestyle including “medical management” of weight loss (but little mention how to fix the food?)
- Risks and questionable benefit of insulin and sulfonylurea
- Post prandial glucose important
Missing
- Specific nutrition intervention including effects of carbs if IR
- More of same language that insulin resistance is “caused” by weight gain (blame patient)
- Need to restrict calories and exercise more (this has failed too many times)
- This is all really complex, especially the meds. There is a term called “Minimally Disruptive Medicine” gaining traction. Look it up if curious.
Some real world DM reversal strategies below:
For an interesting read from a Family Doc changing the world in Northern Europe read here
http://www.dietdoctor.com/diabetes
Canadian Nephrologist Dr. Jason Fung trying to keep his patients off dialysis through better food
https://intensivedietarymanagement.com/
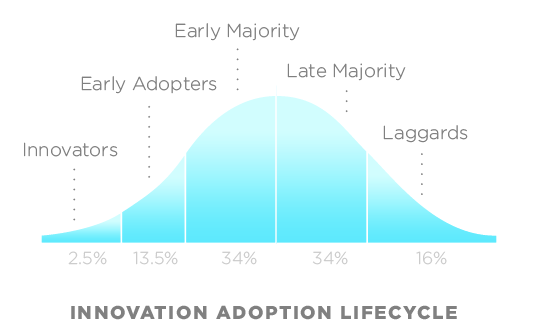
Finally sharing this adapted from a link sent to by NRC colleague Jim Hixson:
Check out Rodgers “Diffusion Adoption of Technology” and you’ll probably agree that low carb advocates can be seen as early adopters, but a vast majority of physicians are far to the right on the bell curve. One’s place on the curve, especially in the beginning of a change, is much more dependent upon mindset, which is strongly influenced by social conformity, and rarely by a logical appreciation of a rational argument. Many ideas never move beyond innovators and early adopters.
The information in this post is not an “experiment”. We are merely replicating what works in metabolic clinics the world over and has through generations.
Keep reading and learning….I sure am. Enjoy
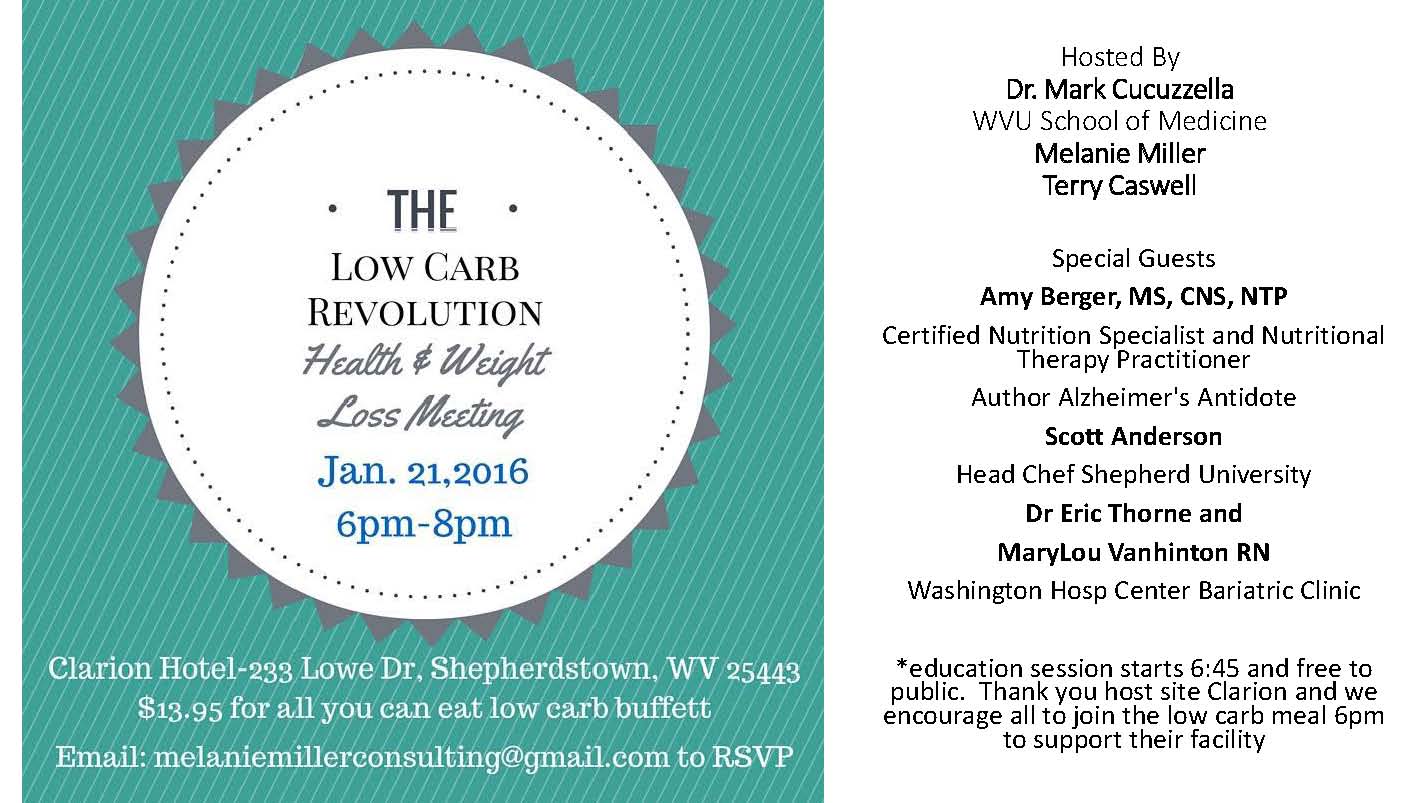
If you are near West Virginia join us Thursday
http://naturalrunningcenter.com/2015/12/17/carb-revolution-west-virginia/
Mark

Great summary and lots of other links to follow up.
I’m a T1 myself and recently adopted a low carb-high fat diet, moderate protein. My blood glucose control has never been better and I feel great as well. A three egg omelette for breakfast, no bolus and a BG or 6.0 mmol/l afterwards.
The most encouraging thing was my annual Consultant’s review at the hospital where I was expecting a “you can’t do that” approach, but got the exact opposite, a doctor astute enough to see the numbers, understand the science and say “it seems to be working for you, so I wouldn’t suggest you change. The group studies do not apply to individuals.”
David thanks for sharing. yes the “free foods” for T1DM are the healthiest (eggs, meat, cheese, leafy greens). you only have 5g of sugar in your bloodstream so for a T1DM trying to manage meals w 60-100g carbs is not possible. Share you knowledge w others
Mark
Hi Mark,
As you know, I have been a T1 diabetic for over 25 years as well as a marathon runner and endurance cyclist. About 5 years ago I adopted a ketogenic (ultra-low carb, high fat, moderate protein) diet and have been consistently in nutritional ketosis ever since. My blood sugar control has never been better (A1C < 6.0) and my insulin requirements have been cut in half (about 20U total per day).
Interestingly, now that I rely on fat as my primary fuel source, I am no longer susceptible to "bonking" toward the end of long workouts. I have done 100+ mile bike rides in which my companions are continuously eating carbs to stay loaded and I am fine the entire time on a little cheese and nuts. A great side benefit!
Owen Faris
thanks Owen for sharing your story….keep the health going for you and your family. 20u insulin a day….folks shoot up this much before a meal and often crash a hour or two later needing to re-sugar. we know this is bad for the cells.
Thanks, Dr Mark.
On Monday of this week I experienced a significant heart attack, resulting in quite a bit of damage–leaving my heart at 30% pumping capacity. I am just starting my road to recovery.
I intend to follow my cardiologist’s instructions while I heal, but I notice a lot of their literature regarding nutrition is dated.
Would the information you are discussing apply even to someone like me who has experienced this kind of event?
I am 6’2″, 180 lbs, was active as a runner, and am 52 years old. The diagnosis was a heart attack involving left anterior descending coronary artery.
Steve Hailstone
Steve I do not want to give advice over email on condition like this but read the works of Dr David Ludwig and Robert Lustig and find the root cause of your CAD. you are young and need to figure out “why”. screen for pre Diabetes.
Thank you, Dr Mark. I left out that there is family history of CAD on my Dad’s side. I will look up those sources and discuss possible pre Diabetes.
Dr Mark. You are correct. There is sign of pre-diabetes. That is very good to know. I have also checked out Dr Lustig’s “Fat Chance” and watched “Fed Up” with my family. Thanks for those resources.
Can you point to any resources on recovery and returning to activity post heart attack? I realize it is a long road, but would appreciate educating myself while I have down time.
Thanks. Steve
thanks Steve. reverse the causes and this is individual. diet is huge as is stress. need a good person to help assess your future risk. make sure you do not have insulin resistance and if you do reverse it w low sugar/starch. this is often the elephant in the room
Hi Mark i am slim active healthy 56 yr old woman who’s been lchf for 3-4 yrs after test showed fbg 5.4 (UK). However although I keep under 75g carb I still show glucose spikes up to 8-9 when I occasionally happen to eat bread or even beans and it’s still highish after 2-3hrs. I have loads fresh veg and a moderate amount of dairy, meat fish. My fbg is still 5.3-4! Dread to think what it would be if I ate ‘normally’! What’s going on? Have I down regulated insulin producing factors or am I infact a prediabetic despite being sporty and thin all my life?
Audrey you need to see someone. you at least have pre Diabetes which is insulin resistance. there is a movement there http://phcuk.org/ to identify and reverse. maybe one of these docs are near you