Dr Mark Cucuzzella and special guest Dr Nicholas Norwitz
Key words: metabolism, therapeutic carbohydrate restriction, low-carb, keto diet
Friends, many of you have seen U.S. News and World Report (USNWR) diet ranking for 2021. This year, there were 39 diets on the list. The ‘Keto Diet’ came in second to last place overall, and in dead last place for health.
Of the 38 other “diets,” several are processed food substitutes requiring monthly subscriptions, and even more are supported by a grand total of zero published randomized clinical trials. It would be laughable and dismissible if not for the fact that so many – including doctors and other healthcare workers – turn to USNWR for what they believe to be reliable and unbiased rankings and reporting for things such as hospitals and colleges.
https://health.usnews.com/best-diet/best-diets-overall
Is this ranking justified?
I wrote this rebuttal last year after similar conclusions.
http://naturalrunningcenter.com/2020/01/09/bestworstdiets2020/
To clarify “keto” would more appropriately be referred to as a “metabolic state,” not a “diet.” Ketosis occurs when fat is burnt as the primary fuel source. This is because some fat needs to be transformed into molecules that are digestible by the brain, i.e. ketones. Ketosis is a natural and completely healthy state (not to be confused with diabetic ketoacidosis), and one could argue the optimal state if you are the spectrum of insulin resistance, a spectrum that includes the majority of Americans. Obesity, Type 2 diabetes, fatty liver, many lipid abnormalities are manifestations of insulin resistance.
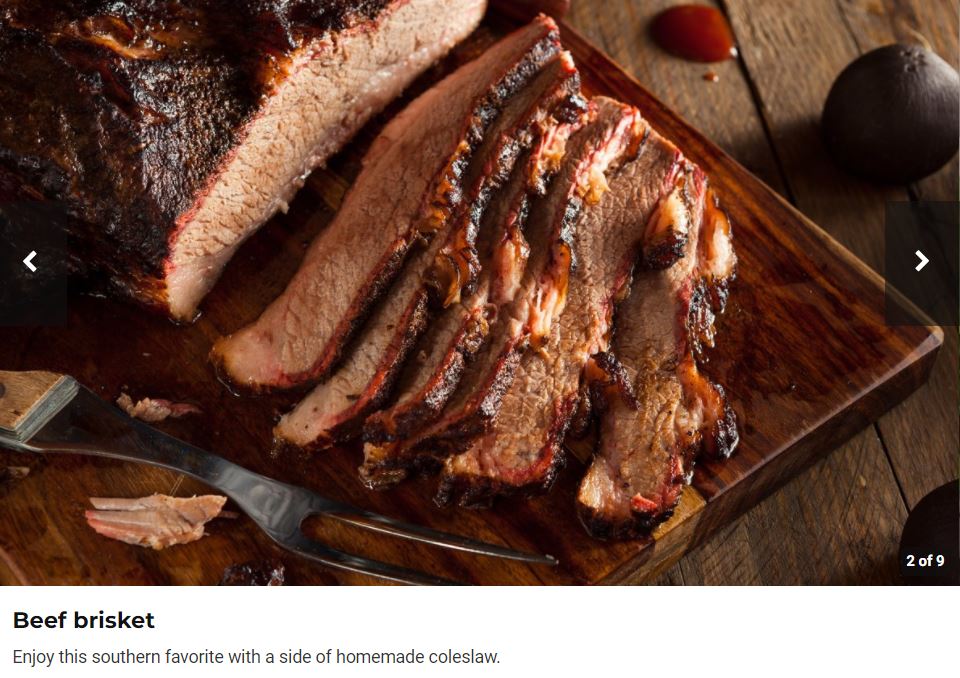
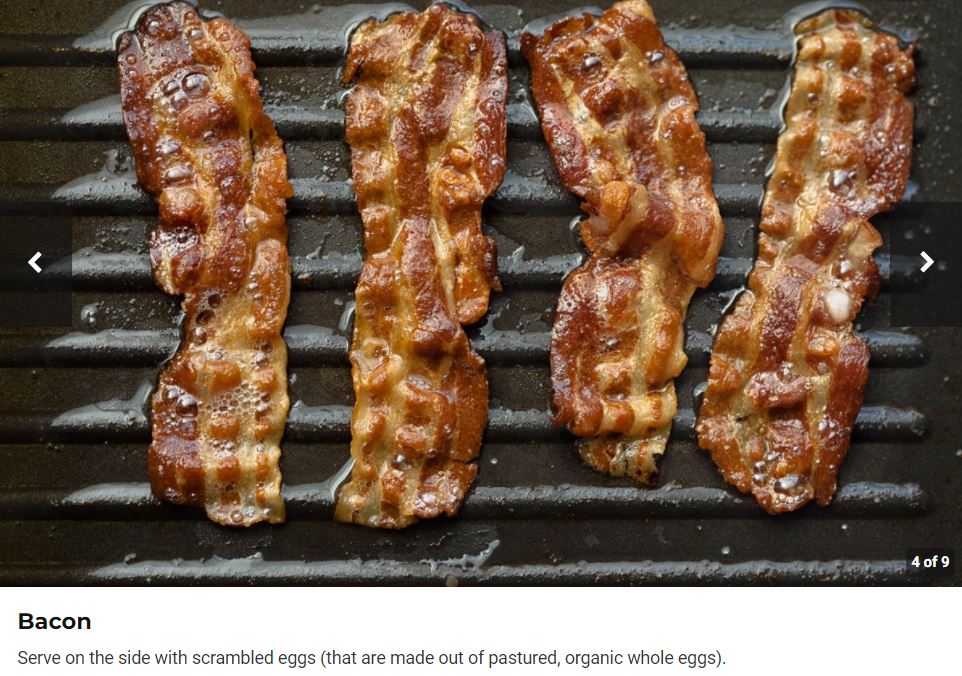
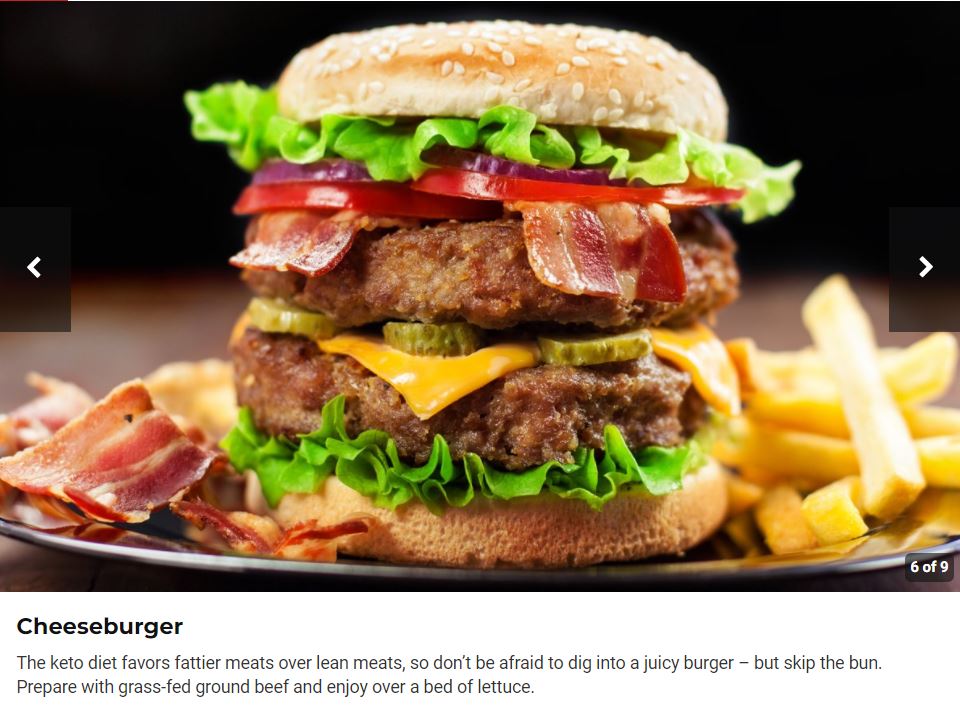
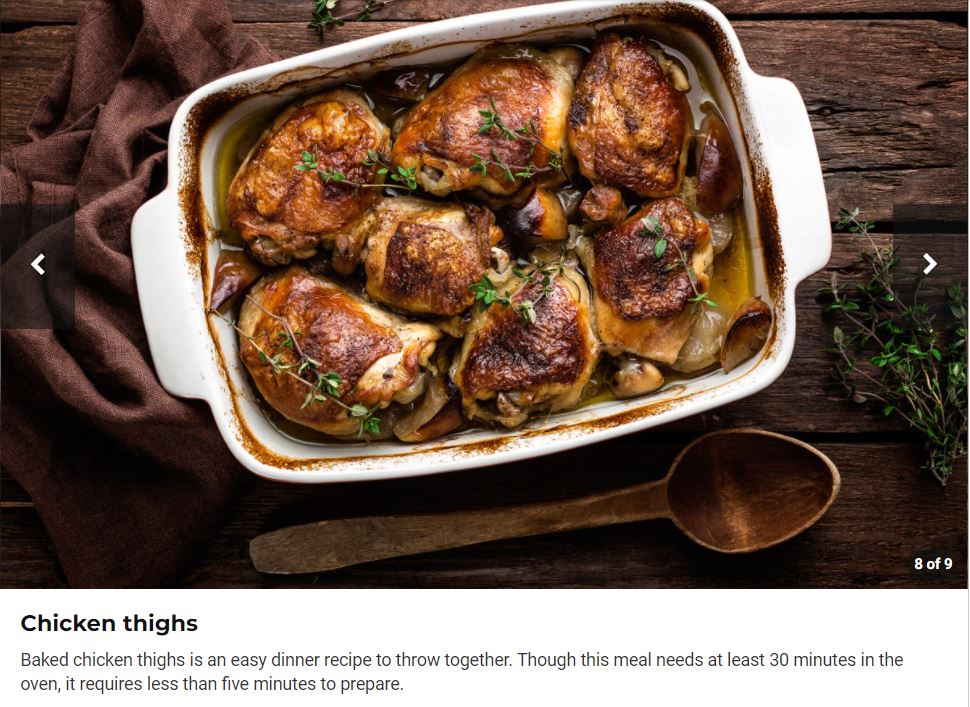
Bizarrely, while the USNWR made some misleading statements about keto — including (i) “These diets provide fewer carbs than is recommended by government guidelines”(Correction from the Institute of Medicine: “The lower limit of dietary carbohydrate compatible with life apparently is zero, provided that adequate amounts of protein and fat are consumed.” IOM (2002)) and (ii) “it is still too soon to tell whether people maintain long-term weight loss from ketogenic diets (Correction, that’s clearly false) – the overall description is actually complementary and the pictures of the food you would eat are nutrient dense and delicious. See the gallery below from the article 🙂
The description does not vilify saturated fat, nor say anything negative about cholesterol, nor imply a keto “diet” is a carnivore diet. It does admit keto is excellent for weight loss and can be maintained and may help improve or prevent brain conditions like Parkinson’s and Alzheimer’s. I would have been nice had they commented on diabetes reversal and referenced the clinical studies showing low-carb ketogenic lifestyles are the best for reversing diabetes, but let’s give them some credit for a reasonable description. So why did it get ranked in dead last for health? It almost seems as if the ranking was post-hoc to the literature review, even if the literature review was biased.
Moving on, you would think that a criteria for any dietary advice is preventing and reversing chronic metabolic dysfunction, which afflicts 88% of our adult population (I wrote about it here)
This year further research and clinical experience validate therapeutic low-carb diets for obesity, diabetes, and metabolic illness. It is hard to find a valid study on any of the ways of eating ranked above this one when it comes to a meaningful outcome (actual disease reduction versus a biomarker such as LDL cholesterol). Worse is extreme weight loss through starvation approach followed by weight gain, drained financial resources, and mental and physiologic destruction. The perfect example would be the Biggest Loser diet which came in ahead of low carb.
I commented on one such recent BMJ review article in the BMJ here.
Also a few highlights from 2020:
A ray of hope for the future of health is amazing work of faith, perseverance, and the desire to heal from colleague, Dr. David Unwin, a GP in the UK. His six-year study showed…
-46% drug-free T2 diabetes remission.
-Significant
improvements in weight, blood pressure and lipid profiles.
-93% remission of prediabetes.
-£50,885 annual saving on the Norwood GP practice NHS diabetes drug budget.
-If every GP practice in England spent the same on drugs for diabetes per
patient as Norwood the NHS could save
£277,000,000
-Older patients can do as well as
younger ones with a low carb approach.
-The participants who started with the worst blood sugars saw the greatest
improvements in diabetic control
-Total weight loss for the 199
participants was 1.6 metric tons (over 3,500 pounds)
-Teamwork from the entire staff and a culture that low-carb should to be offered to all as an option.
https://nutrition.bmj.com/content/bmjnph/early/2020/10/21/bmjnph-2020-000072.full.pdf
And if you have concern about low carb and cholesterol here is the 2-year result from Virta Health:
“Consumption of a very low carbohydrate diet with nutritional ketosis for 2 years in patients with type 2 diabetes lowered levels of small LDL particles that are commonly increased in diabetic dyslipidemia and are a marker for heightened CVD risk. A corresponding increase in concentrations of larger LDL particles was responsible for higher levels of plasma LDL-C. The lack of increase in total LDL particles, ApoB, and in progression of CIMT, provide supporting evidence that this dietary intervention did not adversely affect risk of CVD.”
Impact of a 2-year trial of nutritional ketosis on indices of cardiovascular disease risk in patients with type 2 diabetes
https://cardiab.biomedcentral.com/articles/10.1186/s12933-020-01178-2
This follows their 2 year study in type 2 diabetes remission
On the saturated fat issue (fats found naturally in meat , eggs, and dairy) the Journal of the American College of Cardiology, an institution which has been like the Alamo in its defense on the restricting saturated fats, exonerated them in a recent State-of-the-Art Review. What was extraordinary in this article were the authors, 3 former members of the DGA committee. But a call to action to the DGA committee was sadly ignored as shared by the BMJ.
Even the American Diabetes Association’s own consensus report acknowledges: “Reducing overall carbohydrate intake for individuals with diabetes has demonstrated the most evidence for improving glycemia and may be applied in a variety of eating patterns that meet individual needs and preferences.”
Yes, lets repeat- “The MOST evidence.”
Source: http://care.diabetesjournals.org/content/42/5/731.long
The expanding popularity of low-carb and keto is also telling. If something was not enjoyable, too expensive, inaccessible, dangerous, or simply did not work, it would not continue to grow in acceptance. And this way of eating has a long history even dating back to the pre-insulin days. (note this is the 100th year anniversary of the amazing discovery by Banting and Best). Here is a humbling blog by one of the authors and friend Andrew Koutnik on the history.
So, it’s curious that in the same magazine the low-carb way of eating is again the most popular for many years ongoing. https://health.usnews.com/health-news/blogs/eat-run/slideshows/10-most-searched-diets-of-2020-on-google
A well-formulated low-carb diet has more supporting evidence for conditions of obesity, diabetes, and other conditions of metabolic health than any other way of eating. It is in our DNA to “eat plants and animals.” I am trying to think of a single downside to trying this approach if you are afflicted with metabolic disease. And the beneficial effects are INDEPENDANT OF WEIGHT LOSS.
For the curious here are some databases.
On-line libraries of low carb studies
Diet Dr https://www.dietdoctor.com/low-carb/science
200 references on low carb 1797-2019 https://www.neslazeno.cz/references/
Virta list of research
https://blog.virtahealth.com/low-carb-research-comprehensive-list/
Low Carb Action list of research
http:// https://lowcarbaction.org/low-carb-studies-list/
Metabolic Multiplier 2500 refs
https://www.zotero.org/groups/2384096/metabolic_multiplier/library
……………………………………………………………………….
Now for another ray of help. Here is the writing of 25-year old medical student and scientist
| Nicholas Norwitz, PhD. Watch a video of his work and mission here |
Nicholas is an MD/PhD student having completed for his PhD at Oxford and now doing his MD at Harvard. He is also a Boston Marathon finisher, on crutches!
I am privileged to be a contributor to his new metabolic health cook book coming out this year.
Nicholas models the brave new clinician willing to do the hard science and clinical work to displace established dogma with an approach to restore health.
Nick’s New Book Page: https://ketodietapp.com/books/new-mediterranean-diet
Note, pre-orders up-rank it on Amazon and help bump down calorie counting low-fat style books
Three selected peer-reviewed papers:
1. Keto Diet & Lipid Panel:https://pubmed.ncbi.nlm.nih.gov/32351962/
2. Keto Diet Mental Health: https://journals.lww.com/co-endocrinology/Abstract/2020/10000/Ketogenic_diet_as_a_metabolic_treatment_for_mental.5.aspx
3. Alzheimer’s and insulin resistance: https://pubmed.ncbi.nlm.nih.gov/31417394/
He’s also active on Twitter @nicknorwitz and his new video has spun out into a YouTube channel upon popular demand.
Listen to Nick on Low Carb USA podcast
………………………………………
By Nicholas Norwitz
Not a Fad Diet
The keto diet is often brushed off as a fad diet, but nothing could be further from the truth.
The keto diet is so named because it relies on carbohydrate restriction to shift the body’s metabolism into a fat-burning mode, a state in which the liver also turns some fat into molecules called ketone bodies.
This shift to a fat- and ketone-dependent metabolism was central to our evolution as a species. During evolution, our species underwent periods of food deprivation, and plentiful stores of carbohydrates were rarely available. But, while the body can only store about 450 Calories as freely available carbohydrate energy in the form of liver glycogen, our fat stores are nearly unlimited. Even a relatively lean person has 100,000 stored fat Calories.
Ketosis is a state in which the potential to use those fat Calories to fuel the body and, in particular, the brain is maximized. The “fad” diet gets its name from the fact that we now know about ketone bodies.
The keto diet is just a rebranding for the oldest human diet.
Therapeutic carbohydrate restriction
Admittedly, our goals in the 21st century are distinct from our goals thousands of years ago. Famine is less of an issue and feasting is the danger. In this new environmental context, does the keto diet have any place?
The short answer is, “Yes.” Today the most daunting ongoing medical challenges in the United States are metabolic disease, including obesity, diabetes, heart disease, metabolic syndrome, and Alzheimer’s disease. By mid-century, the number of people living with each diabetes and Alzheimer’s in the United States is projected to triple.
The keto diet has a broad potential to aid what ails us.
The benefits for certain diseases, including obesity and diabetes, depend primarily on Therapeutic Carbohydrate Restriction (TCR). The keto diet is, by nature, a low-carb diet. Decreasing carbohydrates in the diet prevents spikes and drops in the hormone insulin. These spikes and drops, colloquially termed “the insulin roller coaster,” drive a form hormonal hunger in which the body is tricked into desiring food (usually in the form of carbohydrates) not to fulfill a nutritional need but to quench a craving.
This is one way in which the diet can be an excellent weight loss tool. It erases the insulin roller coaster to decrease maladaptive hunger while simultaneously adapting the body to relying on its own fat as a fuel source.
Furthermore, reducing carbohydrates and diminishing the insulin roller coaster improves insulin resistance, a fundamental pathology in type II diabetes. It’s unsurprising that multi-year studies have demonstrated the keto diet is an excellent option for reversing diabetes. (1, 2)
Importantly, to gain the weight loss and diabetes reversing benefits of keto, one need not necessarily go all-in.
While a proper keto diet definitionally requires ketone bodies to rise above a certain level, most laypeople don’t practice keto in this way. Therapeutic Carbohydrate Restriction is a spectrum and patients struggling with conditions that would benefit from TCR should be encouraged to find a carb-appropriate diet for their needs.
The benefits for other diseases, mental illnesses and neurological diseases, may also depend on ketone bodies themselves. These biomolecules are not only clean and efficient sources of fuel but potent signaling molecules. They bind receptor on and within cells, alter enzymatic pathways, and even change the way our genetic code is expressed. Through these signaling mechanisms, ketones alter metabolism to improve the fundamental pathologies (like oxidative stress and inflammation) that generally underly metabolic diseases.
Unwarranted fear of cholesterol
The final defense of those who feel most comfortable sticking with the status quo nutritional advice is often that low-carb diets, which are necessarily high in fat, can increase levels of “bad” LDL cholesterol. Firstly, this happens only in a minority of individuals, although it does happen. More importantly, suffice it to say this defense reveals an outdated-understanding of cardiometabolic health.
For a deeper dive into cholesterol, please see the appendix.
Since when was nutrition actually as simple as you are what you eat?
For example, you might think that eating more saturated fat in place of carbohydrates would increase the saturated fat in your blood. As a matter of fact, it doesn’t. A randomized crossover controlled trial – the gold-standard for nutrition research – demonstrated that when participants ate a high-fat, low-carb diet they ended up with far less saturated fat in their blood than when they ate an isocaloric lower-fat, higher carb diet. This was despite that fact that on the low-carb diet they ate 2.5-times more saturated fat (3).
Even were saturated fat artery-clogging, these and other data strongly suggest it’s the butter, not the bread, that should remain on the table.
Here’s another important question. How is the status quo nutritional advice working for us?
The weight of the evidence
The U.S. News and World Report article states “enthusiasm outpaces evidence.” The insinuation that low-carb and ketogenic diets lack a strong evidence base, as compared to other diets ranked higher on the list, is – quite frankly – a lie.
The report’s rankings demonstrate a lack of understanding of metabolism and an ignorance of the evidence. For example, the Biggest Loser Diet is ranked in the middle of the list, seventeen positions above the keto diet. The former results in a slowing of metabolic rate and leaves an obesogenic fingerprint on the individual, as do most crash diets. Maybe that’s why there are no Biggest Loser reunions. By comparison, carbohydrate restriction can protect or increase metabolic rate (4), and is proven to be sustainable when properly formulated.
A survey of the evidence is telling. While there are dozens of randomized controlled trials on low-carb and ketogenic diets, the majority of which find strong positive benefits, there are a sparse few for vegetarian or vegan diets and zero for other diets on the list, like the Noom diet or Dr. Weil’s diet. That’s not to disparage these diets. It’s simply to say that, in terms of evidence base, there is no stronger diet than a keto diet.
Conclusion
The keto diet is a form of Therapeutic Carbohydrate Restriction with proven benefits for weight loss and a wide range of metabolic diseases. It’s put down because of a misunderstanding of the fundamentals of biology and the scientific evidence base.
While diet is individual, and a keto diet might not be for everyone, keto and other forms of Therapeutic Carbohydrate Restriction should be provided as an option for obesity and metabolic disease, especially because a vanishing small number of Americans are metabolically healthy.
There is no medicine without metabolism.
Appendix Nick’s cholesterol blog
Cholesterol – Corrupted by the Dark Side?
Even if you’ve never seen Star Wars, we’ve bet you’ve heard the soundtrack “The Imperial March.” Not sure? (Click on the link to Imperial March). This ominous tune is Darth Vader’s theme song (you’ve heard of him, right?), and it’s meant to strike fear into the hearts of all who hear its rhythmic beat. Well, for most health-conscious people, the word “cholesterol” evokes the same ominous feeling. But, spoiler alert, just like Darth Vader, cholesterol is a misunderstood villain. In the Star Wars saga, Darth Vader begins life as Anakin Skywalker, a young boy full of potential for good. It is only when external dark and insidious forces, creatively named “the dark side,” corrupt good Anakin Skywalker that he becomes bad Darth Vader. The same is true of cholesterol! Cholesterol (or, more specifically, LDL cholesterol) starts life healthy as good but can be turned bad if we don’t resist the dark side.
Now, if you’re not a fan of Star Wars or otherwise didn’t like our little hook, no worries. The analogy ends here and was simply meant to make the point that cholesterol is good – essential, actually – and it is dark forces, i.e. dark “metabolic circumstances” that corrupt cholesterol and turn it into a biomolecule associated with atherosclerosis and heart disease. In this post, we are going to explain to you what cholesterol actually is and what it’s good for, what “metabolic circumstances” turn cholesterol to the dark side, and what you can do to improve your cholesterol and lipid panel.
What is Cholesterol?
Cholesterol is a molecule that looks sort of like the Olympic rings in which one ring was knocked off. You can get some cholesterol from your diet, but the vast majority is made by your liver (and brain cells, for that matter). Your body makes cholesterol because it’s an essential precursor to hormones like testosterone, estrogen, vitamin D, as well as to the bile acids that help you digest fat. It’s also an essential component of cell membranes and a building block for the brain! Without cholesterol, you’d literally drop dead in an instant.
Clarifying terms: LDL, HDL, and triglycerides
If you’ve ever gotten a basic cholesterol test (we hope you have), then you’ve also probably heard these terms: LDL, HDL and triglycerides. The first thing you should know is that none of them are cholesterol. LDL is “low-density lipoprotein,” a particle containing cholesterol, and HDL “cholesterol” is “high-density lipoprotein,” a particle containing cholesterol. Neither LDL nor HDL are themselves cholesterol, but little spherical molecular boats. These boats also contain a fatty fuel for the peripheral organs of the body (like skeletal muscles and the heart) called “triglycerides.” Typically, it’s LDL that’s perceived to be the heart disease-causing villain. HDL is accepted to be anti-atherogenic (good) and high HDL levels are preferable. Triglycerides are fat fuel and low triglycerides in the blood are a marker of good metabolic health.
Aside: Why do carbs, not fat, increase triglycerides in the blood?
Carbs are stored in your liver as glycogen. However, the carb storage tank is very small and usually remains relatively topped off. But your body isn’t going to just waste carby fuel that you so graciously provided it. Thus, it needs to store the carbs in another form: triglycerides!
De novo lipogenesis is the process by which carbs in the liver are turned into triglyceride fat. These new fat molecules can’t be stored well in the liver (although too many carbs can force this to happen, leading to fatty liver disease). So, the newly created triglycerides need to be shipped off in very low-density lipoprotein (VLDL) boats to storage sites around the body (like those love handles and spare tire!).
The hormone, insulin, increases when you eat carbs. In turn, insulin increases the expression of genes coding for de novo lipogenesis proteins and increases the production of triglyceride-filled VLDL particles by as much as 300%!
So that’s why carbs, not fat, really spike your triglycerides.
And here’s the kicker: de novo lipogenesis mostly produces saturated fat — you know, that type that everyone says will clog your arteries. In fact, we pretty much guarantee that your blood levels of saturated fat will be lower if you substitute carb calories for butter calories.
LDL – The young and the good subverted to the dark side
So, now that we’ve clarified our main terms, let’s focus on the controversial topic of LDL. Most people think it’s “bad cholesterol” but that’s not true. LDL is Anakin Skywalker, a good guy who only turns bad if he is allowed to age and become corrupted. Let’s unpack that statement with an analogy that’s more relatable for those who don’t like science fiction. LDL is like a boat that transports two types of cargo through the bloodstream: cholesterol and triglycerides (fat fuel) from the liver to organs around the body that need building blocks and fuel. LDL boats are created and shipped out from the liver “harbor” as young, big, and fluffy “good” molecules. In a metabolically healthy body, LDL drops off its cargo around the body and then returns to port at the liver, where it’s taken back up. (In this circumstance, only young, good LDL exists, and Anakin is never allowed to become Darth Vader.) But this process can go horribly wrong if the sea is choppy and full of glaciers! When the body is subjected to the metabolic conditions of oxidative stress and inflammation (choppy seas and glaciers), LDL boats get damaged, can’t return to the liver, and sink to the bottom of blood vessels. This LDL shipwreck contributes to the buildup of plaques and heart disease.
The science of plaque build up
(Nerd alert! You can skip this parenthetical paragraph if you’re not scientifically inclined, but we’d be remiss if we didn’t reveal that the situation is a lot more complicated than the choppy seas and glaciers analogy can communicate.
First of all, it may be more accurate to say that the glaciers in the analogy are sugar. Sugar increases in your blood when you have carbs, and these sugar molecules attached to the ApoB lipoprotein on LDL particles in a process called “glycation.” ApoB is supposed to act like a passport to let LDL back into the liver, but glycation breaks this passport, forcing LDL to linger in the blood. High sugar levels go hand-in-hand with oxidative stress, inflammation, and insulin resistance. They are all part of the same complex of “metabolic disease” pathology.
Oxidative stress and inflammation also cause damage to artery walls. Older and Vader-like small, dense and/or oxidized LDL particles can get inside the wall and eventually end up in a clot that we call a plaque. With continued oxidative stress and inflammation, the plaque can build until it breaks off and causes a heart attack or, more rarely, simply occludes the entire blood vessel.
In fact, it gets even more complicated still. There’s speculation that damaged small, dense and/or oxidized LDL doesn’t actually get into blood vessel walls from the inside, or lumen, of the vessels but from the outside. Some evidence suggests that oxidative stress and inflammation inside blood vessels cause the small “vasa vasorum” vessels that themselves supply blood vessels to grow inward and deposit LDL cholesterol from the outside (Subbotin V. 2016).)
Oxidatives stress, inflammation, and insulin resistance
The point is this: LDL doesn’t cause heart disease, the “metabolic circumstances” of oxidative stress, inflammation, and insulin resistance do. Unfortunately, about 88% of Americans have at least one of the markers of metabolic syndrome (Araujo J. et al. 2019)! The features of metabolic syndrome, which indicates poor metabolic health and confers an increased risk of obesity, diabetes, Alzheimer’s, other dementias, cardiovascular disease, and so on, include (i) having a high waist circumference, (ii) higher fasting glucose, (iii) high blood pressure, (iv) high triglycerides, and (v) low HDL. (Interesting, triglycerides and HDL, but not LDL are among the criteria. Hmm?) Clinical criteria aside, the point we are trying to make is that the “metabolic circumstances” of oxidative stress, inflammation, and insulin resistance that cause metabolic syndrome at the molecular and cellular levels (the dark side, if you will) are the norm. Therefore, is it really any surprise that LDL levels are correlated – in some but not all epidemiological studies (more on that below) – with heart disease? It doesn’t surprise us. Plus, correlation does not show causation. And, when you look at LDL (and total) cholesterol in context, LDL’s villainy is diminished.
For example, when HDL is high and triglycerides are low – a marker of good metabolic health – LDL levels become almost irrelevant. For example, one study found that if HDL was high (above 57 mg/dL) and triglycerides were low (below 97 mg/dL), incidence of heart disease as about 5%, irrespective of LDL levels (above or below 170 mg/dL). But, if HDL was low and triglycerides were high, incidence of heart disease jumped to about 12%, again, irrespective of LDL levels (Jeppesen J. et al. 2001). An easy number to remember is if you can get an triglyceride/HDL ratio of 1 or below, you get a gold medal (you placed in the cholesterol Olympics, wink)! Furthermore, analyses that “subfractionated” LDL into young, big, healthy “Anakin” particles, and old, small, dense “Vader” particles, reveal that it’s only the small, dense particles that are associated with cardiovascular disease (St-Pierre A. et al. 2004; Hoogeveen RC. et al. 2014). In fact, on a ketogenic diet, it may be better to have higher big LDL because you’ll be burning primarily fat as fuel (Norwitz N and Loh V. 2020). Remember: LDL boats carry fat fuel.
Furthermore, when the epidemiology is examined broadly, the association between total cholesterol and LDL and heart disease dissipates. For example, a systematic literature review published in the British Medical Journal examined the findings of 19 different studies that included 68, 094 people above the age of 60 and explored the relationship between LDL cholesterol levels and death by cardiovascular disease or any other cause. They found that that most studies reported no association between LDL levels and death by cardiovascular disease. Actually, there were only two exceptions, and these found that lower LDL levels were associated with higher cardiovascular-related mortality. Whoops! Furthermore, the majority of the evidence suggested that lower LDL levels predicted higher rates of overall death. Yikes! The authors state directly that “elderly people with high LDL-C live as long or longer than those with low LDL-C” (Ravnskov U. et al. 2016). See, we told you there was more to the story. Certainly, there is still debate among experts, but, if nothing else, you should know that there is controversy and that the historical perception that LDL-C is bad is teetering.